It is feasible for a single-practitioner podiatry practice to add weight bearing CT (WBCT) imaging and realize economical…
WBCT Indication Series: Hallux Valgus
Hallux Valgus
Hallux valgus is a three-dimensional deformity of the first ray in which the first metatarsal moves into varus, pronates, and dorsiflexes. This deformity affects the 1st metatarsophalangeal (MTP) joint and is often accompanied by significant functional disability & foot pain.
A weight bearing CT scan can:
• Assess rotation (pronation) of the 1st metatarsal.
• Assess the position of the sesamoids and degenerative changes at the metatarsosesamoid joints.
• Assess congruency and degenerative changes at the 1st MTP joint.
• Assess instability, degenerative changes, and rotational changes at the 1st tarsometatarsal (TMT) joint in three planes.
Diagnosis
While radiographs are typically sufficient to make the diagnosis, WBCT scans may be useful to plan surgical treatment.
Treatment Planning
Because hallux valgus is a three-dimensional deformity, a three-dimensional, weight bearing imaging modality can assist in planning surgical indications and correction.Surgeons can better determine where along the medial column the deformity should be addressed.
Regardless of procedure chosen, a WBCT scan can provide guidance on the degree of rotational correction of the 1st metatarsal, evaluate instability at the 1st TMT joint, plan for adequate reduction of the sesamoids, and assess congruency of the 1st MTP joint. Changing rotation of the 1st metatarsal and adequate reduction of the sesamoids have been shown to result in improved patient-reported outcomes and decreased recurrence rates1,2.
Postoperative Assessment
For postoperative assessment of hallux valgus treatment, a WBCT can:
• Accurately assess adequacy of correction3.
• Accurately assess healing in the 1st TMT joint4.
• Accurately assess sesamoid position as plain radiographs cannot determine whether the sesamoids have been reduced within their grooves5.
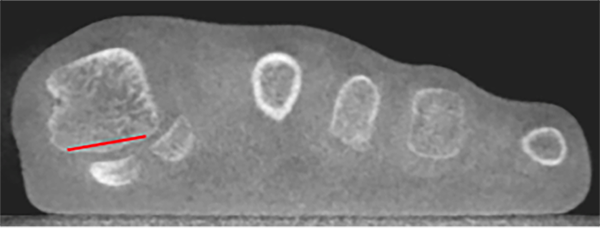
Evaluation of Deformity
16 yo female with a family history of hallux valgus who presents with pain in her left forefoot.
WBCT scan demonstrated mild pronation of the first metatarsal (red line), sesamoid subluxation, and instability at the 1st TMT joint (yellow lines).


Postoperative Evaluation
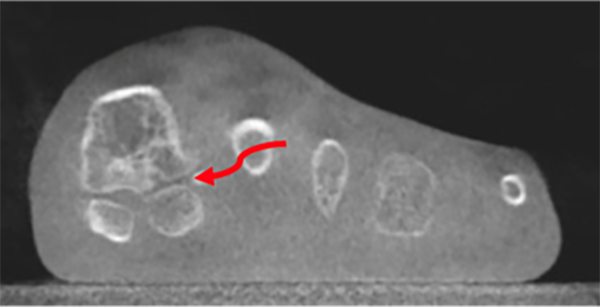
58 yo female who underwent a 1st TMT joint fusion for hallux valgus.
WBCT scan demonstrated degenerative changes at the metatarsosesamoid joints and reduction of the sesamoids (red arrow) and bony bridging across the 1st TMT joint (yellow arrow).



Dr. Scott Ellis, MD
Dr. Scott J. Ellis is an Orthopedic Surgeon at HSS. He is an expert in reconstructive surgery of the foot and ankle and in addition to seeing patients, he conducts research focused on improving surgical outcomes.
Click Here to get direct links to the latest studies using WBCT scans.
(1) Association of First Metatarsal Pronation Correction With Patient-Reported Outcomes and Recurrence Rates in Hallux Valgus. Conti et al. FAI 2022.
(2) Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. Okuda et al. JBJS 2009.
(3) Jasper, Ryan & Mallavarapu, Vineel & Stebral, Hannah & Jones, Matthew & VandeLune, Christian & Schmidt, Eli & Talaski, Grayson & Fayed, Aly & Carvalho, Kepler & Kim, Ki Chun & Mansur, Nacime Salomao & Dibbern, Kevin & de Cesar Netto, Cesar. (2022). Three-dimensional assessment of hallux valgus correction using the Lapicotton technique. Journal of the Foot & Ankle. 16. 237-241. 10.30795/jfootankle.2022.v16.1674.
(4) Steadman J, Sripanich Y, Rungprai C, Mills MK, Saltzman CL, Barg A. Comparative assessment of midfoot osteoarthritis diagnostic sensitivity using weightbearing computed tomography vs weightbearing plain radiography. Eur J Radiol. 2021 Jan;134:109419. doi: 10.1016/j.ejrad.2020.109419. Epub 2020 Nov 21. PMID: 33259992.
(5) A New Measure of Tibial Sesamoid Position in Hallux Valgus in Relation to the Coronal Rotation of the First Metatarsal in CT Scans. Kim et al. FAI 2015.