Orthopedic decision-making depends on accurate representation of anatomy—particularly when joint alignment and bone relationships change…
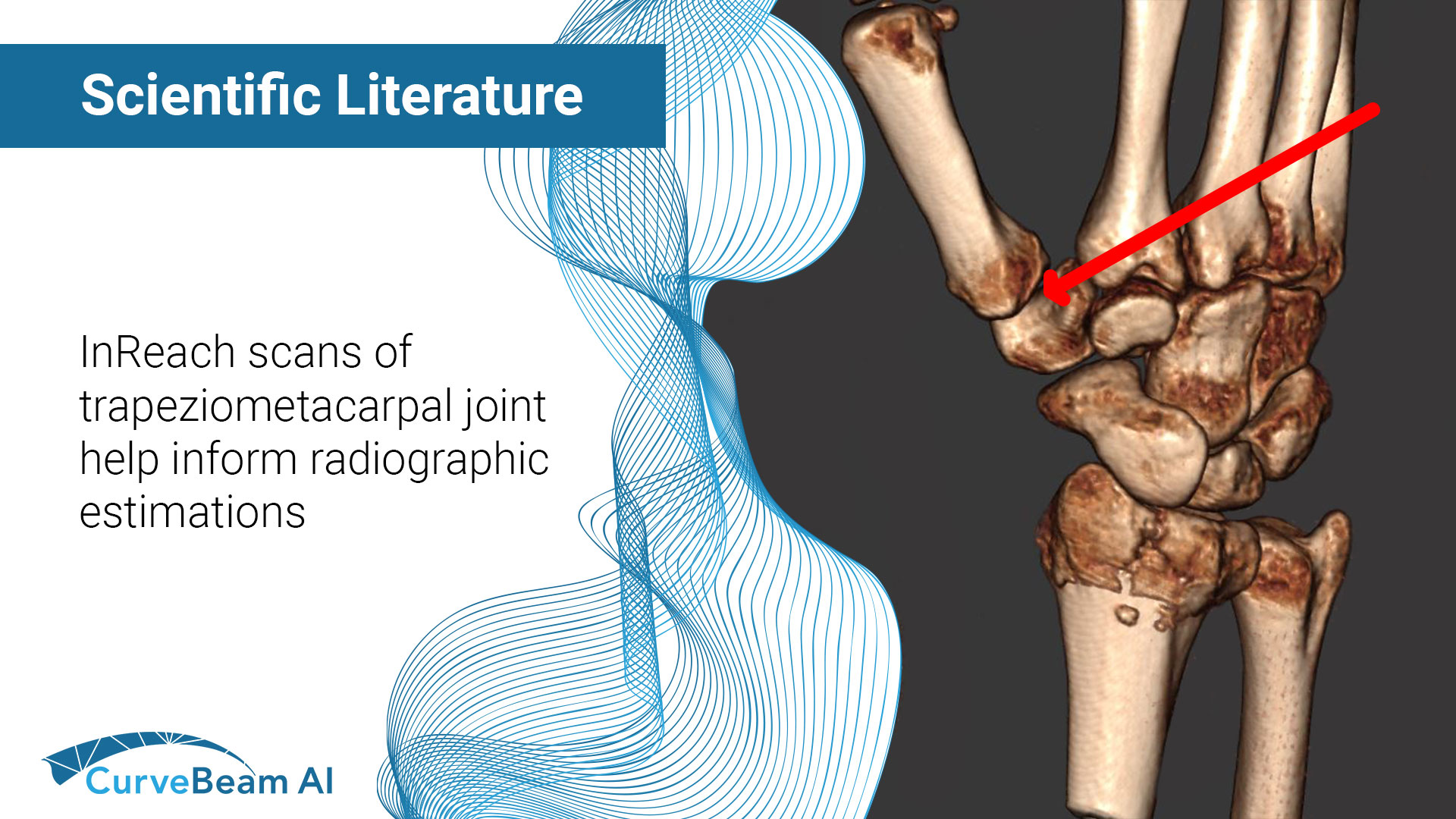
Estimation of Radiographic Joint Space of the Trapeziometacarpal Joint with Computed Tomographic Validation
Key Points:
- Cone Beam Computed Tomography (CBCT), a three-dimensional (3D) imaging modality, can readily evaluate complex joint structures.
- The most important radiographic (X-Ray) criterion used in surgical decision making for osteoarthritis is joint space narrowing (JSN), or the loss of joint space width (JSW).
- The developed methodology has potential for automated and accurate X-Ray measurement of trapeziometacarpal (TMC) JSW.
The TMC joint, at the base of the thumb, is the most affected joint of the wrist. Currently, plain X-Ray is the most common imaging method used to evaluate musculoskeletal disorders in the wrist, such as osteoarthritis. Scoring systems such as the Kellgren-Lawrence classification provide criteria to determine how progressed osteoarthritis in the hand is via X-Ray. However, quantifying parameters can be challenging due to the spatial complexities of two-dimensional (2D) projections of 3D joints.
Computed tomography (CT) is an imaging modality that allows for evaluation and quantification of the complex TMC joint structure and JSW in 3D. Although X-Ray is more readily available, CT can have greater analytic capabilities.
Researchers at the University of Arizona Hand Research Laboratory aimed to develop a method to measure radiographic joint space of a healthy TMC using a “correction factor” based on data from CT cadaveric studies. They hypothesized that X-Ray based TMC JSW would underestimate CT-based TMC JSW.
CT scans from a CurveBeam AI InReach were taken of 15 cadaveric hands whose four fingers were secured around a cylinder in a grasping orientation. Nine (9) specimens’ thumbs were positioned in a neutral position with no external manipulation and six (6) were positioned with an approximate 45 degree of extension. The reconstructed anatomy and simulated X-Ray images (posterior-anterior view) were then generated using CurveBeam AI’s post-processing software CubeVue.
The CT-based and X-Ray based measurements of JSW were 3.61 ± 0.72 mm and 2.18 ± 0.40 mm, respectively.
On the CT, researchers identified a single 3D feature on the articular surface of the 1st metacarpal and approximated a corresponding standardized location on radiographs, based on the arc length of the projected articular surface of the 1st metacarpal.
They used this data to devise a correction factor that could be applied to radiographs to better estimate actual JSW.
The correction factor for radiograph-based joint space was 1.69 ± 0.41. Before correction, the difference between the CT-based and X-Ray based joint space was 1.43mm [95% CI: 0.99 − 1.86 mm; p < 0.001]. After correction, the difference was −0.11 mm [95% CI: −0.63 − 0.41 mm; p ¼ 0.669].
Researchers concluded that the corrected measurements of X-Ray TMC JSW agreed well with the CT-measured JSW. With in-vivo validation, the developed methodology has potential for automated and accurate X-Ray measurement of TMC JSW.
Further validation utilizing in-vivo imaging from a larger sample size would strengthen the standardization and improve the accuracy and applicability of the developed X-Ray TMC JSW measurement method.
To read the full study click here.